
Main causes of pathology
- wear high heels;
- Carry a bag or backpack on one shoulder and do not carry it alternately;
- Sleeping or resting in an uncomfortable position for long periods of time;
- Sedentary work;
- weightlifting.
- Previous injury to the musculoskeletal system;
- curvature of the spine;
- flatfoot;
- Congenital hip dislocation or subluxation;
- autoimmune diseases;
- Inflammation of joint tissue;
- Pathology of the circulatory system;
- endocrine diseases;
- obesity.
Lumbar osteochondrosis: symptoms
- Pain in the affected area of the spine;
- Pain radiating upward to the shoulder blade area or downward to the pelvis and hip joint;
- A persistent feeling of tension in the lower back;
- Difficulty bending and turning;
- slouch;
- limp;
- Muscle weakness or, conversely, increased tone;
- Tingling sensation.

stage of disease
- Stage one. The first structural and functional changes begin. The discs become dry and may rupture. Symptoms at this stage are mild. Many patients mistakenly believe they are tired after a long day at work, wearing uncomfortable shoes, or exercising. The main symptom of early-stage osteochondrosis is mild discomfort in the lower back that worsens with bending and turning. There may be mild pain that subsides with rest.
- The second stage. The height of the intervertebral discs decreases and the bone structure becomes closer. This can trigger a new wave of symptoms - stiffness and pain when moving. The pain becomes persistent and severe and may radiate to the pelvis and legs.
- The third stage. During this stage, the vertebrae become deformed. Formation of a herniation - the disc bulges into the spinal canal area, but the annulus fibrosus remains intact. The main symptoms are severe pain that is disturbing even at rest, decreased sensitivity, a crunching sound when moving, tingling and numbness in the lower back.
- The fourth stage. Pathological changes continue to progress. Loss of function of the vertebrae. Hernia form. Osteophytes (bone growths) form. Blood vessels may be squeezed and nerve fibers may be pinched. Against the background of worsening blood circulation, the function of the pelvic organs is disturbed. In men, the risk of erectile dysfunction is increased, and in women, disruption of the menstrual cycle is observed. Advanced osteochondrosis presents with severe low back pain, claudication, impaired mobility or even complete inability to move, and elevated body temperature.
pathological form
- Low back pain. It's a sharp stabbing pain that makes it impossible to move. The pain may be caused by pinched nerves or muscle spasms.
- Lombardinia. It’s a long-lasting, heart-wrenching pain. It is characteristic of the stages of herniation and hernia formation. Additionally, discomfort may be related to ligament sprains.
- Sciatica. This is a severe pain that radiates into the pelvic area. Patients complain of pain when walking, sitting, or changing body positions.
- Radiculopathy. It is accompanied by compression of nerve endings due to vertebrae deformation. With this disease, sensitivity is reduced and the affected area becomes numb. Shows soreness and tingling. Decreased muscle tone, impaired reflexes, and tingling in the legs may occur.
- Discogenic lumbar osteochondrosis. This is a serious condition in which the patient's movements are restricted. His lower back and limbs were numb. Other symptoms include general weakness, fever, involuntary urination, and, if the condition persists, weight loss.

Risks of spinal disease
- intervertebral hernia;
- Inflammation of the sciatic nerve;
- Radiculitis;
- Paresis.
Pathological diagnostic methods
- MRI;
- radiography;
- Contrast myelography;
- Multi-slice CT.
Lumbar Osteochondrosis: Treatment
Lumbar Osteochondrosis: Physical Therapy Approaches
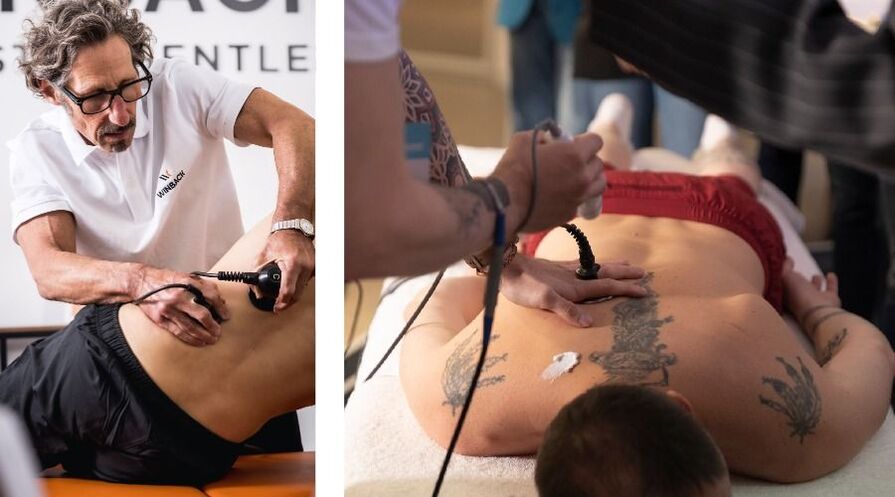
- Electrophoresis - exposing problem areas to sustained electrical pulses and topical medications may be used;
- Dynamic therapy - a variation of electrotherapy using pulsed electric current;
- Magnetic therapy – treatment using alternating or static magnetic fields;
- Ultrasound therapy – the effects of high-frequency sound waves;
- Shock wave therapy - exposure to low-frequency sound pulses;
Lumbar osteochondrosis: drug treatment
- NSAIDs (systemic and local) suppress inflammation of the vertebrae and adjacent tissues;
- Muscle relaxants to relieve muscle spasms;
- Vasoprotectants improve blood circulation;
- Chondroprotectant, protects intervertebral disc cartilage tissue from damage;
- B vitamins improve nerve conduction;
- Painkillers used to treat severe pain that limits mobility.
Exercise therapy as a treatment for sacral and lumbar regional pathologies
- Work out with a trainer. The trainer will show you which exercises are allowed in a given situation and ensure they are performed correctly. Even the smallest technical flaws can significantly reduce the effectiveness of training and even cause injury.
- Prepare lessons carefully. Before exercising, it is recommended to warm up the muscles - you can gently massage the lower back and sacrum.
- Strict dosage. The lower back is a vulnerable area. To avoid overexertion, you need to monitor the duration of your sessions. Their optimal duration is no more than 20 minutes.
- Gradually increase exercise intensity. For inexperienced beginners, simple exercises and short procedures are suitable. For those who have been doing exercise therapy for a while, you can move on to more sophisticated options.
- Remember to be regular. A one-time workout won't lead to noticeable improvements. Pain in the lumbar and sacral spine is reduced if the patient undergoes exercise therapy regularly (ideally twice a week).
- Consider contraindications. Physical therapy has been shown to be a safe method of treating osteochondrosis, but it does have limitations. You should stop exercising if you feel unwell: have a fever, weakness, or an elevated temperature.
- in the acute phase. Only smooth and slow movements are allowed. If the pain gets worse during exercise, you need to stop and let the joint rest.
- In the subacute stage. The pain syndrome subsides and mobility returns, so the intensity and duration of training can be slightly increased. However, to avoid deterioration, you need to monitor your health carefully.
- In remission. We allow a full range of exercises for lumbar spine pathology, but it is important to remember that overexertion can lead to new exacerbations of the disease.

manual therapy
- Eliminates excessive tension in muscle fibers;
- pain relief;
- Restores blood supply to the lumbar and sacral areas;
- Improves metabolic processes.
surgical method
- Endoscopic herniectomy - using microsurgical instruments and a built-in camera;
- Transfacet resection of intervertebral hernia - using a neurosurgical tube dilator;
- Laminectomy – surgical removal of pathologically altered bony prominences;
- Microdiscectomy – eliminates hernia.
disease prevention
- Arrange your workplace properly during office work. The chair back should support the lower back and the table should be at the right height.
- Avoid wearing uncomfortable shoes. The optimal heel height for women is 5 cm. It is also recommended to exclude flat shoes as they can lead to foot deformation and flat feet - this is one of the factors.
- Risk of osteochondrosis.
- exercise. Lifting heavy objects should be avoided. Swimming, walking and aerobic exercise are all useful if there are no contraindications.
- Eat a balanced diet. Foods that must include calcium, phosphorus and B vitamins in your diet include fish, dairy products, green leafy vegetables and grains. These substances are needed to strengthen all parts of the joints and support the nervous system.
- Make sure you get enough sleep. It’s best to sleep on a medium-firm orthopedic mattress. It will provide anatomically correct posture, insulating the body from daily stress.
- Control your weight. Obesity is one of the predisposing factors. If the weight is normal, the load on the spine is adequately distributed and the risk of circulatory diseases is minimized.






























